What You Should Know About Aortic Surgery
Aneurysms
Summary:
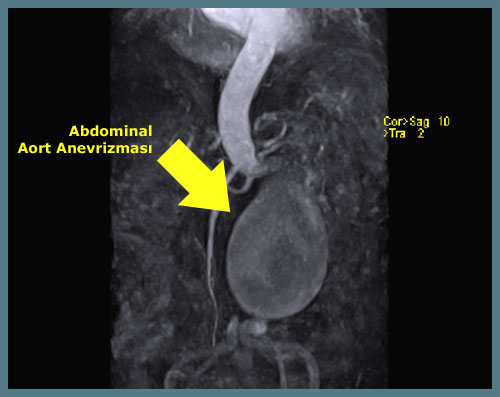
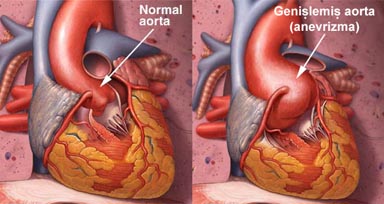
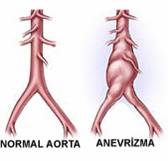 An aneurysm is a permanent dilation or ballooning of the vessels. Aneurysms most frequently develop in the aorta, the largest artery in the body. Over time, the aneurysm enlarges, and if left untreated, it may rupture and often lead to death. Most aneurysms cause no symptoms and are discovered incidentally during examinations for other reasons. If detected early, aneurysms can be permanently treated. The classical treatment is to surgically replace the enlarged segment of the artery with an artificial graft. Another less invasive option is placing an internal stent graft through catheters into the aneurysmal segment.
An aneurysm is a permanent dilation or ballooning of the vessels. Aneurysms most frequently develop in the aorta, the largest artery in the body. Over time, the aneurysm enlarges, and if left untreated, it may rupture and often lead to death. Most aneurysms cause no symptoms and are discovered incidentally during examinations for other reasons. If detected early, aneurysms can be permanently treated. The classical treatment is to surgically replace the enlarged segment of the artery with an artificial graft. Another less invasive option is placing an internal stent graft through catheters into the aneurysmal segment.
More Information:
An aneurysm is a permanent dilation or ballooning of the vessels. It most commonly occurs in the aorta. Without treatment, it may rupture and often results in death. Aneurysmal rupture ranks as the 13th leading cause of death in the general population.
Some individuals are at higher risk for aneurysms:
- People over the age of 60,
- Those with a family history of aneurysms,
- Smokers,
- Individuals with peripheral vascular disease,
- Those with high blood pressure,
The risk of aneurysm increases with age and is more common in men.
Cause:
The exact cause of aneurysm is not fully understood. However, damage to the proteins collagen and elastin—which help maintain the strength of the vessel wall—leads to weakening of the artery and subsequent dilation. This condition is frequently associated with atherosclerosis (hardening of the arteries).
Symptoms:
Most aneurysms cause no symptoms. Some individuals may notice a pulsating mass in the mid-abdominal area. Back pain, abdominal pain, or flank pain may be mistakenly attributed to aging.
However, persistent abdominal, flank, or back pain, especially when accompanied by hypertension, should raise suspicion for aneurysm. Rupture presents with entirely different symptoms.
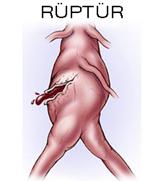
Rupture causes sudden internal bleeding and often results in death. A person with a known or unknown aneurysm who experiences sudden, severe back or abdominal pain along with fainting or blood pressure changes should be evaluated immediately for rupture.
Diagnosis:
If detected early, aneurysms can be permanently treated. Since they often cause no symptoms, they are typically found incidentally. Many can be diagnosed during physical examination. The simplest method for diagnosing aneurysm is ultrasonography. It is fast, inexpensive, and reliable. It is also an excellent screening tool for the general population. All men over age 65 should be screened with ultrasound at least once in their lifetime.



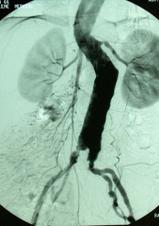
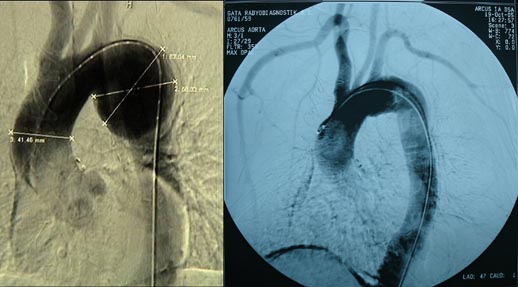
Additional diagnostic methods such as CT, MRI, and angiography may be used to plan treatment. These identify the size (the most critical factor in treatment), location, and relationships to surrounding organs. Angiography is not usually required for open surgery planning but is recommended for endovascular repair.
Treatment:
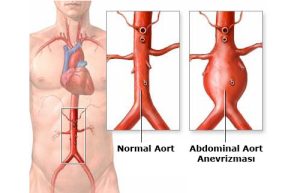
The presence of an aneurysm does not always require surgery. The decision is based on the aneurysm’s diameter and symptoms. The diameter is the most important factor, as rupture risk increases with size. Surgery is generally recommended when the diameter exceeds 5.5 cm (about the size of a large lemon). If the aneurysm is smaller but causing pain or rapidly growing, surgery may also be necessary.
Patients with aneurysms smaller than 5–5.5 cm and without symptoms are monitored with ultrasound or CT every 6 months. Quitting smoking and treating high blood pressure can slow aneurysm growth.
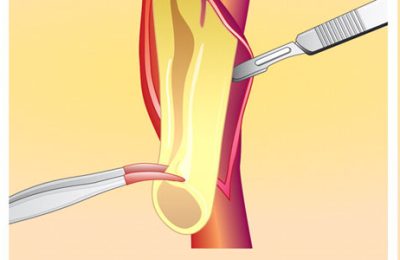
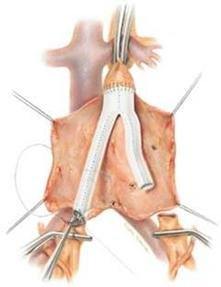
The traditional treatment involves replacing the dilated vessel segment with a synthetic graft. This has been performed for over 50 years and provides durable results. The surgery is performed under general anesthesia with a large abdominal incision. Patients are typically discharged within 7–10 days and recover fully in 1–2 months. This method offers complete cure, though the operative mortality risk averages around 5%.
A less invasive option is to place a stent graft inside the vessel through catheters, known as endovascular aneurysm repair (EVAR). This method has a 10-year history. It is done without opening the abdomen, using small incisions in the groin under X-ray guidance.
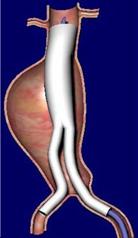
In this method, the artificial graft is inflated at the aneurysm site and fixed internally with hooks. Patients are usually discharged in 1–2 days. However, this method is not suitable for all cases. The aneurysm may continue to enlarge or rupture even after the graft is placed, so periodic CT or Doppler ultrasound follow-up is necessary. Unlike open surgery, EVAR may not provide permanent cure.
Aortic Dissection
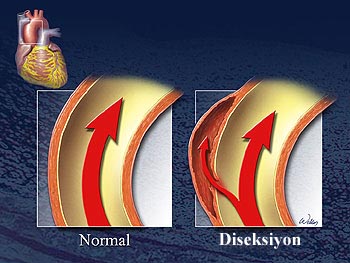
The aorta has three main wall layers. Aortic dissection occurs when the inner layer tears and blood enters the middle layer, creating a second channel. It is more common in the elderly and is a medical emergency. If the outer layer also tears, it can rupture, which is often fatal. 50% of patients die within the first 48 hours. The risk increases by 1% each hour thereafter. Medical treatment alone has a 58% mortality rate. If rupture occurs, survival is extremely unlikely.
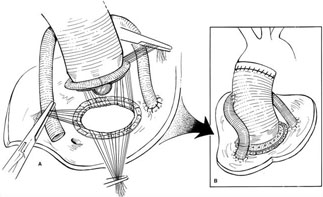

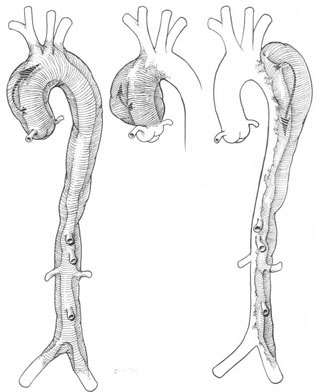
Bentall procedure for ascending aortic aneurysm repair (using artificial aortic valve and graft)
Ascending Aortic Aneurysm
Cabrol procedure for ascending aortic aneurysm repair (using artificial aortic valve and graft)
Types of Aortic Dissection by Location
Pre- and post-operative aorta images of a patient with descending aortic aneurysm operated in our clinic. In this surgery, the heart-lung machine was used, and the patient’s body temperature was lowered to 19°C. Circulation was completely stopped for 30 minutes.
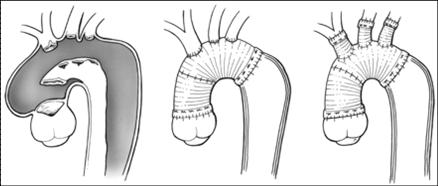
Aortic dissection repair with artificial graft. In such surgeries, the heart-lung machine is used, and the body is cooled to 19°C. Circulation is completely stopped until the surgery is complete.