General Information:
Atherosclerotic plaque can form a bulge inside the carotid artery, reducing blood flow to the brain and sometimes causing clot formation. These conditions may lead to stroke and paralysis. The surgical procedure to remove the inner layer of the carotid artery along with the plaque is called carotid endarterectomy. Numerous studies have shown that carotid endarterectomy is the most effective treatment for preventing stroke and paralysis due to carotid artery stenosis.
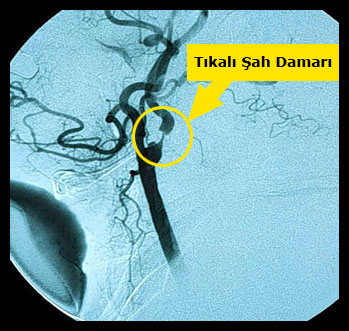
There are two carotid arteries (carotids) on either side of the neck, which carry oxygenated blood from the heart to the brain. Near the level of the jaw, each carotid artery divides into two branches: external and internal. The external carotid artery supplies blood to the face and scalp, while the internal carotid artery enters the skull and nourishes the brain.
As people age, cholesterol and fat in the bloodstream begin to accumulate inside the arterial wall, forming raised areas called plaques. As the plaque enlarges, the artery narrows and hardens. This condition is known as arteriosclerosis or atherosclerosis. Plaques in the carotid artery usually develop at the point where the artery divides into internal and external branches and tend to extend toward the internal carotid. Due to their irregular surfaces, plaques often become covered with clots over time. When this process advances, the artery may become completely blocked, significantly reducing blood flow to the brain and resulting in a stroke.
Furthermore, plaques may rupture, releasing fragments into the bloodstream that can travel to the brain and block smaller vessels. This can cause paralysis, blindness, and speech disorders. These ulcerated plaques pose an even greater risk.
Endarterectomy is performed for plaques that cause significant narrowing and pose a risk of stroke. It remains one of the most commonly performed vascular surgeries.
When is endarterectomy performed?
Endarterectomy should be performed if the narrowing is severe enough to cause a stroke risk and the patient has experienced a transient or permanent stroke, blindness, or speech difficulties.
- – If the patient has had a mild to moderate stroke within the last six months and the carotid stenosis is between 50–69%,
- – If there is severe carotid stenosis (over 80%) without symptoms, surgery is still recommended due to the high risk of future stroke.
In patients undergoing coronary artery bypass surgery due to heart disease, carotid endarterectomy may be performed before, during, or after heart surgery depending on the patient’s condition.
Endarterectomy is not recommended in some high-risk situations:
– Advanced age or serious systemic illness such as advanced-stage cancer,
– Anatomical difficulty or high risk in accessing the carotid arteries,
– Coexisting brain conditions such as aneurysms.
Preoperative Preparation:
Before surgery, tests such as carotid color Doppler ultrasound, magnetic resonance angiography, or conventional angiography are required. It is important that the patient’s blood pressure is well controlled before surgery.

How Is It Performed?
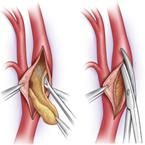
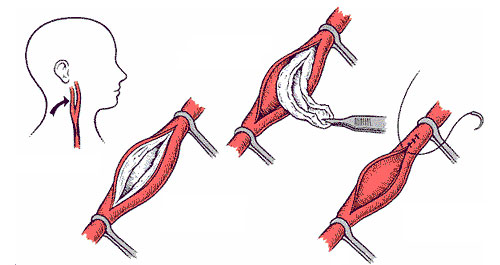
The surgery can be performed under local anesthesia (via neck injection) or general anesthesia (with sedation). After sterilizing the surgical field to minimize infection risk, a 10–12 cm vertical incision is made on the neck to expose the carotid arteries. Great care is taken due to the many nerves and vessels in this area. Heparin is administered to prevent clotting, and the carotid artery is temporarily clamped above and below the narrowing with vascular clamps.
The artery is then opened longitudinally, and the plaque along with the inner arterial layer is carefully removed. If signs of cerebral ischemia arise, a temporary tube called a shunt is inserted to maintain cerebral blood flow. Once the plaque is fully removed, a patch graft is used to close the artery. The clamps are then released, restoring blood flow. The procedure typically lasts 1–1.5 hours, with the artery clamped for approximately 20–30 minutes.

Postoperative Care:
After carotid surgery, the patient stays in the hospital for several days. During this time, brain function, blood pressure, and wound drainage are closely monitored. After discharge, patients should avoid strenuous activity, driving, and seek medical attention if they experience headaches, neck swelling, or changes in neurological function. Most patients return to their normal routine within a few weeks.
Re-narrowing of the artery occurs in about 6% of patients. To prevent this, maintaining ideal weight, avoiding cholesterol-rich and saturated fat foods, exercising regularly, and taking prescribed medications is strongly recommended.
Possible Side Effects (Complications)
Although carotid endarterectomy is an effective treatment to reduce future stroke risk, there is still a 1–3% chance of stroke during surgery. Another possible complication involves injury to neck nerves, which may lead to temporary hoarseness, difficulty swallowing, or restricted tongue movement.
Main Risk Factors That Increase Surgical Risk:
· Severe narrowing or blockage in other arteries supplying the brain,
· Uncontrolled high blood pressure,
· Previous history of stroke,
· Diabetes mellitus




